Loading...


Life After Kidney Transplant
The Wellness Ambassadors have all had transplants
and can guide you on your post-transplant journey.
Protecting Your Transplanted Kidney
Congratulations! You’ve just had a successful kidney transplant. While this is an exciting time, it can also be quite scary. All of the Wellness Ambassadors have been in your shoes, and we are here to help!
The first three months after your surgery are extremely important as a kidney transplant operation is a major operation and the body needs time to heal. Your kidney transplant may not last forever through no fault of your own. We want to help you maximize the long-term survival of your transplant. In general, you should:
- Be seen by your transplant team on a regular basis and follow their advice.
- Take your anti-rejection medications daily in the proper dose and at the right times during the day, to keep your body from rejecting your new kidney.
- Follow the recommended schedule for lab tests and clinic visits to make sure that your kidney is working properly.
- Follow a healthy lifestyle including proper diet, hydration, exercise, and weight loss if needed.
Transplant Timeline
Click on the icons below to view the post-transplant timeline!
1 Week
After surgery, you will spend 5-7 days on average in the hospital to begin your recovery process. The length of time you stay in the hospital will depend on how well the kidney is working and if you have any complications.
These first few days will be a "healing" period. Your belly and side will be sore, and you may experience numbness around the incision area. You’ll also feel tired, which is normal in the beginning stages of your healing. Strength for standing and walking will take a couple days to build back up and you may feel tired as you start your healing.
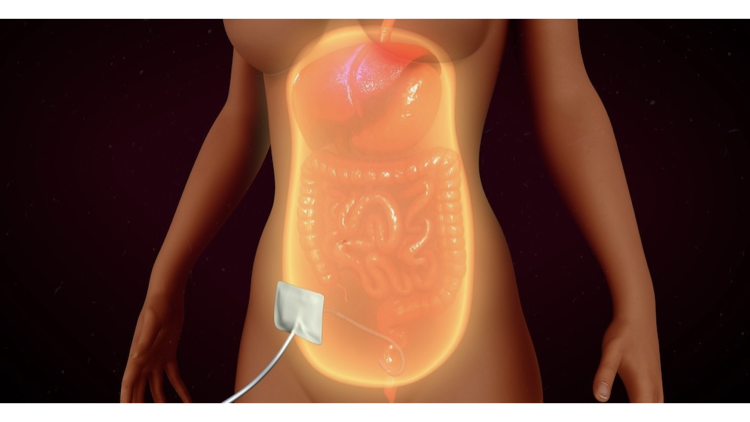
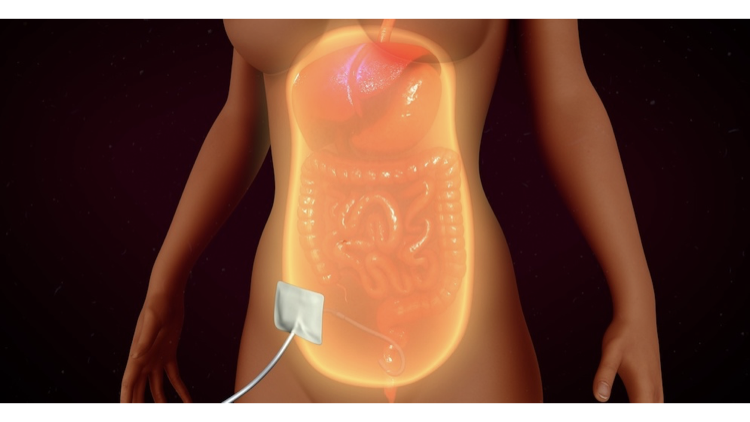
During the transplant surgery, a stent will be placed in the ureter connecting the new kidney to your bladder. The stent helps keep the connection (anastomosis) between the new ureter and your bladder open while the connection heals. The stent may be removed anywhere from 5 to 8 days to up to 6 weeks later. While in the hospital, you will have a Foley catheter that drains the urine from the bladder. It is usually removed before you go home. Some patients may even need to wear a bladder control undergarment temporarily after it is removed.
As your nephrologist checks on you post-surgery, you may still require a few dialysis treatments. Don’t panic! If the kidney does not work immediately after surgery, the dialysis treatments give it time to recover from the whole transplant process. In time, the sessions will cease and you will have a fully functioning kidney.
Your care team will be there to support and monitor you to make sure you’re on the right track to healing. When you are discharged from the hospital, you will receive the necessary information, including a review of medications, diet suggestions, and restrictions you need to know about. You will also be given a supply of your medications and a schedule for your follow-up visits.
1 Month
During the first month, you may experience discomfort navigating around your home, sleeping, standing and walking. This will improve with time. You will need to focus on adjusting to your new medications; consistency with your medications will be vital to the success of your transplant.
For your first month, you will typically visit the clinic twice a week. Your labs will be drawn and you will meet with your nephrologist and physician assistant (PA) or transplant coordinator. They may adjust the prescriptions for your medications and advise you of any concerns. You may see your surgeon sometime during this month to ensure your incision is healing well. These visits are a great time to relay any questions or concerns that you have. Your team is there for you, so be sure to lean on them!
3 Months
By month 3, you should be feeling much better! Doctors’ visits may be less frequent and your medications may be adjusted. You will still be taking some medications for infection prevention beyond 3 months. The swelling and pain in your lower belly should have subsided and your incision site should be healing. You may resume full activity, including exercise and driving.
Some patients may take a little longer to recover strength and resume normal activity or return to work, so do not be discouraged. It is at this point that you should feel more confident in managing your post-transplant care.
1 Year
After one year, most kidney transplant recipients are able to resume “normal” activities and have an overall sense of well-being. Be mindful; you must continue to follow up with your care team and take your medications as prescribed. Even if you are doing well, you may be called in for a kidney transplant ultrasound and biopsy as part of the routine post-transplant management protocol. If there is some question about how the transplanted kidney is functioning, you may also need to have an ultrasound of your kidney, followed by a biopsy. You can ask questions about the reason for any procedure that is being considered.
As a transplant patient, it is very important to maintain a healthy diet and lifestyle, as well as making sure to follow up with your primary care doctor and any other specialists you may need, including mental health services. In addition, don’t be afraid to reach out to family and friends for support as you adjust to your new lifestyle. Your continuing health and wellness depend on you working with your healthcare team; be sure to follow their instructions carefully and don’t be afraid to ask questions. You are on your way to getting your wings back!
After surgery, you will spend 5-7 days on average in the hospital to begin your recovery process. The length of time you stay in the hospital will depend on how well the kidney is working and if you have any complications.
These first few days will be a "healing" period. Your belly and side will be sore, and you may experience numbness around the incision area. You’ll also feel tired, which is normal in the beginning stages of your healing. Strength for standing and walking will take a couple days to build back up and you may feel tired as you start your healing.
During the transplant surgery, a stent will be placed in the ureter connecting the new kidney to your bladder. The stent helps keep the connection (anastomosis) between the new ureter and your bladder open while the connection heals. The stent may be removed anywhere from 5 to 8 days to up to 6 weeks later. While in the hospital, you will have a Foley catheter that drains the urine from the bladder. It is usually removed before you go home. Some patients may even need to wear a bladder control undergarment temporarily after it is removed.
As your nephrologist checks on you post-surgery, you may still require a few dialysis treatments. Don’t panic! If the kidney does not work immediately after surgery, the dialysis treatments give it time to recover from the whole transplant process. In time, the sessions will cease and you will have a fully functioning kidney.
Your care team will be there to support and monitor you to make sure you’re on the right track to healing. When you are discharged from the hospital, you will receive the necessary information, including a review of medications, diet suggestions, and restrictions you need to know about. You will also be given a supply of your medications and a schedule for your follow-up visits.
During the first month, you may experience discomfort navigating around your home, sleeping, standing and walking. This will improve with time. You will need to focus on adjusting to your new medications; consistency with your medications will be vital to the success of your transplant.
For your first month, you will typically visit the clinic twice a week. Your labs will be drawn and you will meet with your nephrologist and physician assistant (PA) or transplant coordinator. They may adjust the prescriptions for your medications and advise you of any concerns. You may see your surgeon sometime during this month to ensure your incision is healing well. These visits are a great time to relay any questions or concerns that you have. Your team is there for you, so be sure to lean on them!
By month 3, you should be feeling much better! Doctors’ visits may be less frequent and your medications may be adjusted. You will still be taking some medications for infection prevention beyond 3 months. The swelling and pain in your lower belly should have subsided and your incision site should be healing. You may resume full activity, including exercise and driving.
Some patients may take a little longer to recover strength and resume normal activity or return to work, so do not be discouraged. It is at this point that you should feel more confident in managing your post-transplant care.
After one year, most kidney transplant recipients are able to resume “normal” activities and have an overall sense of well-being. Be mindful; you must continue to follow up with your care team and take your medications as prescribed. Even if you are doing well, you may be called in for a kidney transplant ultrasound and biopsy as part of the routine post-transplant management protocol. If there is some question about how the transplanted kidney is functioning, you may also need to have an ultrasound of your kidney, followed by a biopsy. You can ask questions about the reason for any procedure that is being considered.
As a transplant patient, it is very important to maintain a healthy diet and lifestyle, as well as making sure to follow up with your primary care doctor and any other specialists you may need, including mental health services. In addition, don’t be afraid to reach out to family and friends for support as you adjust to your new lifestyle. Your continuing health and wellness depend on you working with your healthcare team; be sure to follow their instructions carefully and don’t be afraid to ask questions. You are on your way to getting your wings back!
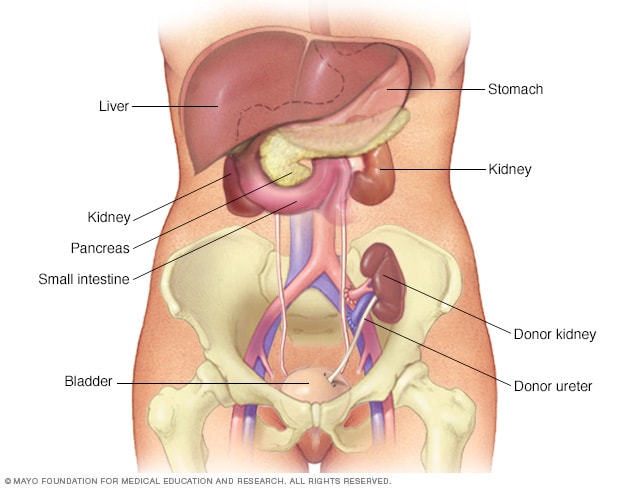
Placement of Your Donated Kidney
Curious about the location of your new kidney? The transplanted kidney is placed in the lower belly on the front side of the body in the pelvis. Placing the kidney in this position allows it to be easily connected to blood vessels and the bladder.
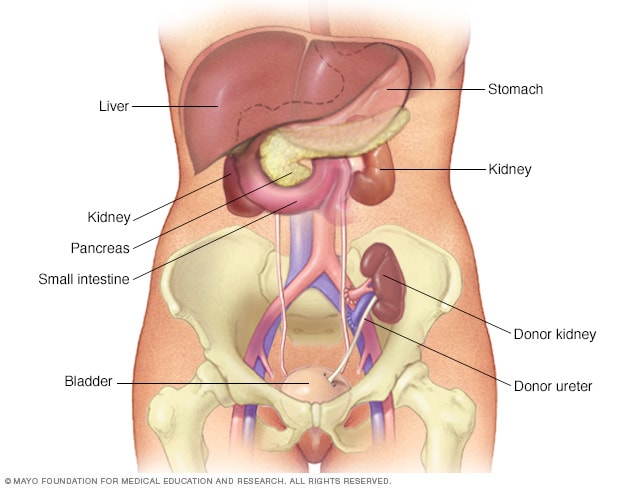
We thank the Mayo Foundation for Medical Education and Research for granting permission to reproduce this image.
Your kidney transplant is one of the most important investments you will make in your lifetime. Below are the best practices to protect it.
Travel
Travel within the U.S. is not recommended in the first 3 months after transplant. International travel is not recommended until after the first year. For those living in populated cities such as New York City, it is recommended that you avoid public transportation for the first 3 months. All of these modes of travel can increase your risk of infection.
Driving
Most patients should not drive until their surgical site is well healed and they are off pain medications and are able to twist and turn easily (typically about 6 weeks after their transplant).
Social
While you may be tempted to celebrate your new transplant, it is critical that you limit your social interactions to smaller groups to avoid contracting any infections and, most importantly, COVID-19. Social events such as concerts, festivals, and athletic games should be avoided.
When You Go Out
Be sure to wear your mask and keep sanitizer handy!
Physical
Your body needs time to heal post-surgery. Your surgeon and transplant team will advise you not to lift anything heavier than 20 pounds in the first 6 weeks after surgery.
Dietary
Visit our post-transplant nutrition page to learn more!
Hygiene
It is recommended you opt for showers instead of baths until your incision site is healed. Avoid rubbing the area directly.
Smoking
Smoking can damage a kidney transplant, and survival of the kidney is worse in patients who smoke. If you currently smoke, it is encouraged you stop. Reach out to your transplant team for resources to help you quit.
Restrictions
While transplantation is optimal for “getting your wings back”, there are restrictions you will need to follow to ensure you remain safe and avoid any complications.
Travel

Travel within the U.S. is not recommended in the first 3 months after transplant. International travel is not recommended until after the first year. For those living in populated cities such as New York City, it is recommended that you avoid public transportation for the first 3 months. All of these modes of travel can increase your risk of infection.
Driving

Most patients should not drive until their surgical site is well healed and they are off pain medications and are able to twist and turn easily (typically about 6 weeks after their transplant).
Social

While you may be tempted to celebrate your new transplant, it is critical that you limit your social interactions to smaller groups to avoid contracting any infections and, most importantly, COVID-19. Social events such as concerts, festivals, and athletic games should be avoided.
When You Go Out

Be sure to wear your mask and keep sanitizer handy!
Physical

Your body needs time to heal post-surgery. Your surgeon and transplant team will advise you not to lift anything heavier than 20 pounds in the first 6 weeks after surgery.
Dietary

Visit our post-transplant nutrition page to learn more!
Hygiene

It is recommended you opt for showers instead of baths until your incision site is healed. Avoid rubbing the area directly.
Smoking

Smoking can damage a kidney transplant, and survival of the kidney is worse in patients who smoke. If you currently smoke, it is encouraged you stop. Reach out to your transplant team for resources to help you quit.
Medication
Anti-rejection medications will be vital for you as they decrease the body’s natural immune response to a “foreign” substance (your transplanted kidney). They will work to suppress your immune system and prevent your body from rejecting your new kidney. After the first few months, you will start to feel much better and may think there’s no need to take the medications any longer because your kidney is functioning. However, no matter how wonderful you may feel, you must stay consistent with your medications to avoid a rejection episode!
Even years later, you should never stop taking your anti-rejection medication, regardless of how great you feel and even if you think your transplanted kidney is working well. Stopping or missing any dose of your medication may cause rejection to occur. Also, be sure to speak with your transplant team before taking any over-the-counter medications, herbal products (including herbal teas, marijuana and related cannabinoid (CBD) products), or medications prescribed by a doctor who is not part of your transplant team.
While your new medications are life-saving and critical for your quality of life, there may be side effects or complications you need to be aware of (see the figures below). Some medications may be required post-transplant to control possible health complications such as high blood pressure, high cholesterol, and diabetes.

Click on the Images to Expand
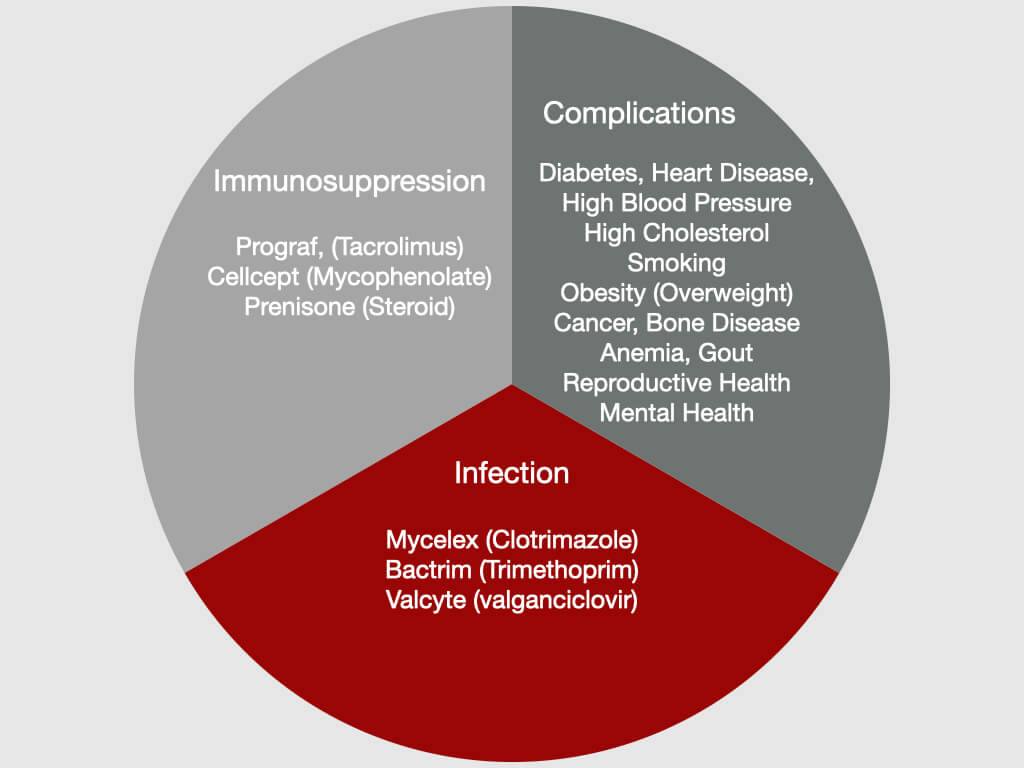
Medications commonly prescribed for the reasons indicated when a transplant patient is discharged and possible complications.
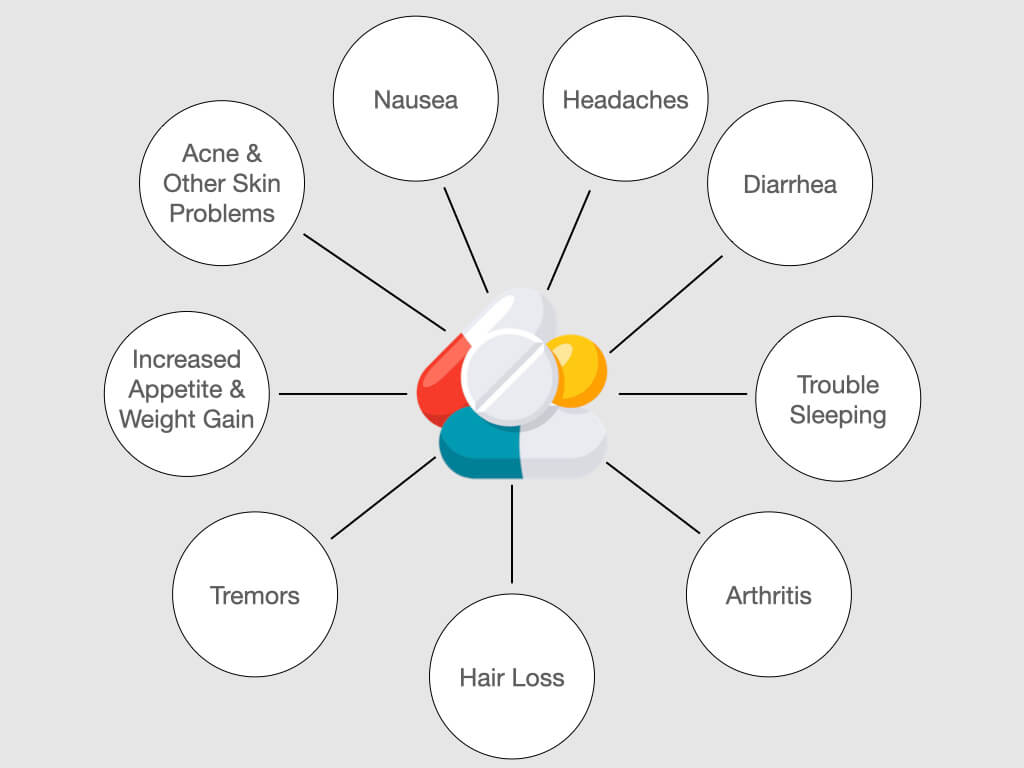
Potential side effects to transplant medications.
Medication

Anti-rejection medications will be vital for you as they decrease the body’s natural immune response to a “foreign” substance (your transplanted kidney). They will work to suppress your immune system and prevent your body from rejecting your new kidney. After the first few months, you will start to feel much better and may think there’s no need to take the medications any longer because your kidney is functioning. However, no matter how wonderful you may feel, you must stay consistent with your medications to avoid a rejection episode!
Even years later, you should never stop taking your anti-rejection medication, regardless of how great you feel and even if you think your transplanted kidney is working well. Stopping or missing any dose of your medication may cause rejection to occur. Also, be sure to speak with your transplant team before taking any over-the-counter medications, herbal products (including herbal teas, marijuana and related cannabinoid (CBD) products), or medications prescribed by a doctor who is not part of your transplant team.
While your new medications are life-saving and critical for your quality of life, there may be side effects or complications you need to be aware of (see the figures below). Some medications may be required post-transplant to control possible health complications such as high blood pressure, high cholesterol, and diabetes.
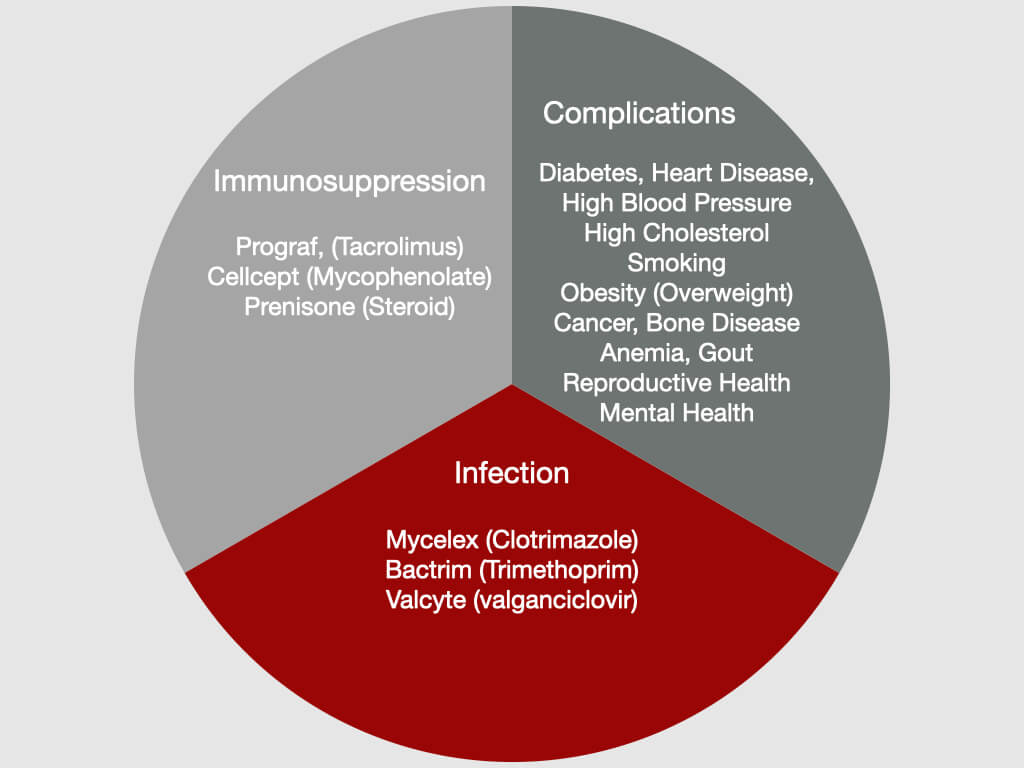
Medications commonly prescribed for the reasons indicated when a transplant patient is discharged and possible complications.
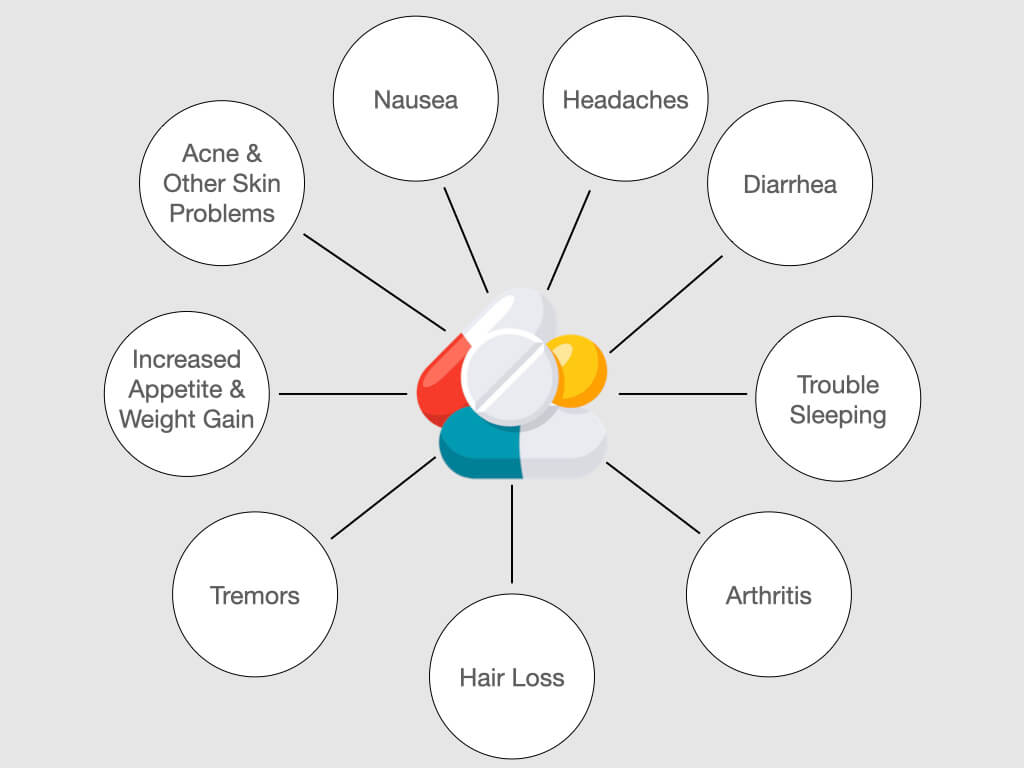
Potential side effects to transplant medications.
Medication
Anti-rejection medications will be vital for you as they decrease the body’s natural immune response to a “foreign” substance (your transplanted kidney). They will work to suppress your immune system and prevent your body from rejecting your new kidney. After the first few months, you will start to feel much better and may think there’s no need to take the medications any longer because your kidney is functioning. However, no matter how wonderful you may feel, you must stay consistent with your medications to avoid a rejection episode!
Even years later, you should never stop taking your anti-rejection medication, regardless of how great you feel and even if you think your transplanted kidney is working well. Stopping or missing any dose of your medication may cause rejection to occur. Also, be sure to speak with your transplant team before taking any over-the-counter medications, herbal products (including herbal teas, marijuana and related cannabinoid (CBD) products), or medications prescribed by a doctor who is not part of your transplant team.
While your new medications are life-saving and critical for your quality of life, there may be side effects or complications you need to be aware of (see the figures below). Some medications may be required post-transplant to control possible health complications such as high blood pressure, high cholesterol, and diabetes.

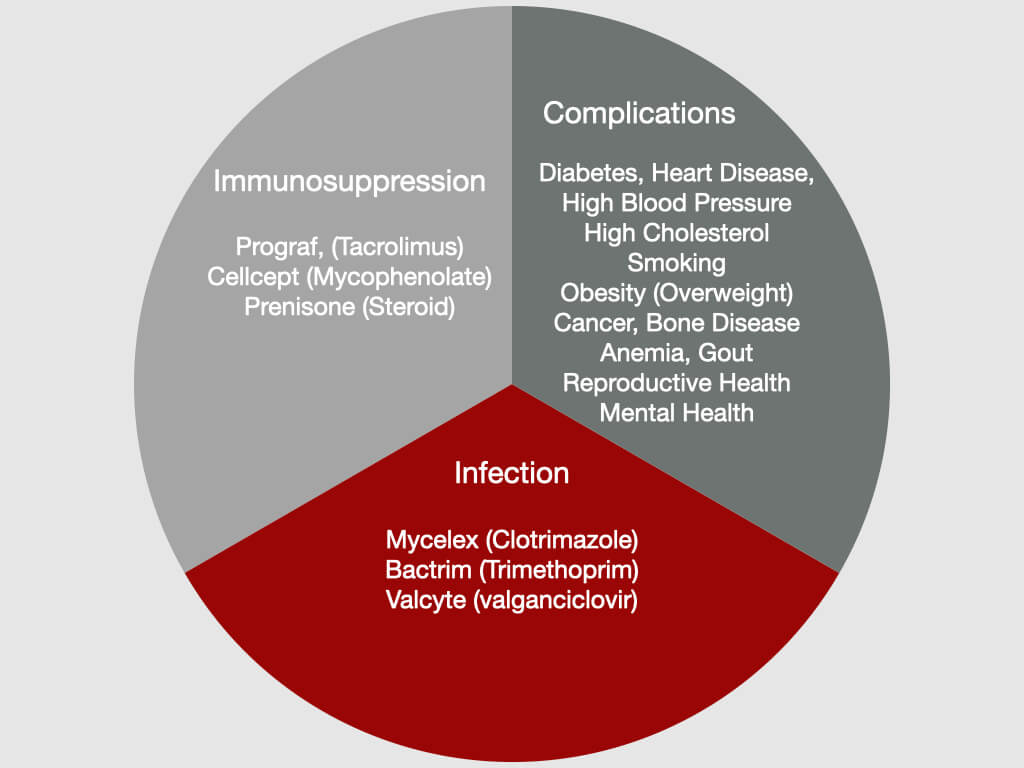
Medications commonly prescribed for the reasons indicated when a transplant patient is discharged and possible complications.
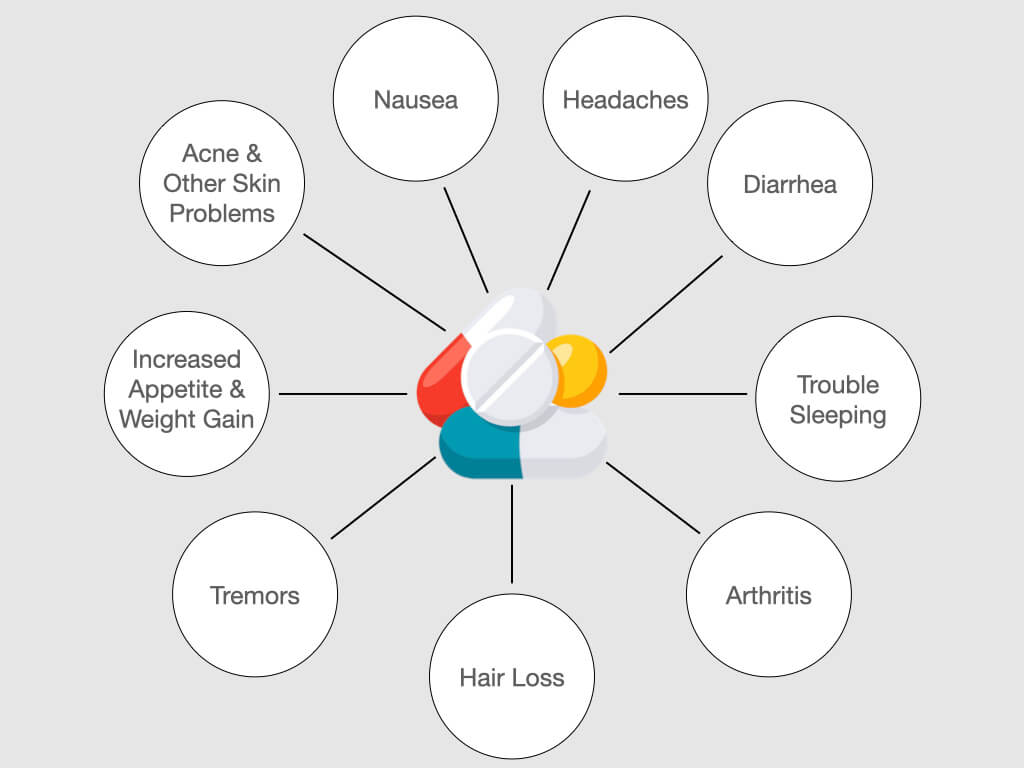
Common side effects to transplant medications.
Rejection
Following a kidney transplant, rejection is a critical complication that can occur. You were not born with your transplanted kidney, so your body will recognize it as a “foreign” object and try to protect you by “attacking” or rejecting it. Your anti-rejection medications help you to combat this; however, you will have to do your part in taking them exactly as prescribed. You can also take other steps to help prevent rejection of a kidney transplant.
Tips to Help Prevent Rejection:
- Take your medication daily! Make it your duty to stay consistent and keep up with any medical changes your team prescribes.
- Continue to wear your mask and avoid being around sick persons and large groups of people. If you haven’t already, get vaccinated and keep up with CDC booster shot recommendations for Immunocompromised persons.
- Follow all dietary restrictions given by your nutritionist. Drink plenty of water to stay hydrated and avoid food high in sodium, fat, and cholesterols.
- With your doctor's clearance, begin a daily exercise routine such as walking, biking, or a dance class. Staying physically active will be a key part in your healing.
- Speak up! Learn about signs of rejection/infection and communicate any concerns you have to your care team. You know your body better than anyone. If something doesn’t feel right, say something!

Following a kidney transplant, rejection is a critical complication that can occur. You were not born with your transplanted kidney, so your body will recognize it as a “foreign” object and try to protect you by “attacking” or rejecting it. Your anti-rejection medications help you to combat this; however, you will have to do your part in taking them exactly as prescribed. You can also take other steps to help prevent rejection of a kidney transplant.
Tips to Help Prevent Rejection:
- Take your medication daily! Make it your duty to stay consistent and keep up with any medical changes your team prescribes.
- Continue to wear your mask and avoid being around sick persons and large groups of people. If you haven’t already, get vaccinated and keep up with CDC booster shot recommendations for Immunocompromised persons.
- Follow all dietary restrictions given by your nutritionist. Drink plenty of water to stay hydrated and avoid food high in sodium, fat, and cholesterols.
- With your doctor's clearance, begin a daily exercise routine such as walking, biking, or a dance class. Staying physically active will be a key part in your healing.
- Speak up! Learn about signs of rejection/infection and communicate any concerns you have to your care team. You know your body better than anyone. If something doesn’t feel right, say something!

Following a kidney transplant, rejection is a critical complication that can occur. You were not born with your transplanted kidney, so your body will recognize it as a “foreign” object and try to protect you by “attacking” or rejecting it. Your anti-rejection medications help you to combat this; however, you will have to do your part in taking them exactly as prescribed. You can also take other steps to help prevent rejection of a kidney transplant.
Tips to Help Prevent Rejection:
- Take your medication daily! Make it your duty to stay consistent and keep up with any medical changes your team prescribes.
- Continue to wear your mask and avoid being around sick persons and large groups of people. If you haven’t already, get vaccinated and keep up with CDC booster shot recommendations for Immunocompromised persons.
- Follow all dietary restrictions given by your nutritionist. Drink plenty of water to stay hydrated and avoid food high in sodium, fat, and cholesterols.
- With your doctor's clearance, begin a daily exercise routine such as walking, biking, or a dance class. Staying physically active will be a key part in your healing.
- Speak up! Learn about signs of rejection/infection and communicate any concerns you have to your care team. You know your body better than anyone. If something doesn’t feel right, say something!

Are there different types of rejection? There are two common types of rejection, cellular and antibody-mediated rejection. Acute cellular rejection involves the recipient's cell attacking the transplanted kidney and acute antibody-mediated rejection involves antibodies formed by the recipient also attacking the kidney. These forms of ‘acute’ rejection typically occur during the first year after transplant but can also occur at any time if anti-rejection medicine is not taken correctly. Acute rejection can often be successfully treated. Chronic rejection typically involves antibodies, formed by the recipient, that will attack the transplanted kidney. It usually occurs slowly over a long period of time and treatment is often unsuccessful.
What are anti-rejection medications? Anti–rejection (immunosuppressant) medications decrease the body’s natural immune response to a “foreign” object (your transplanted kidney). They lower (suppress) your immune system to prevent your body from rejecting your new kidney. You will be taking anti-rejection medication every day after your transplant. There are also some anti-rejection medicines that are only given to treat a rejection episode in a clinic or hospital.
Why do I need to take anti-rejection medication? No matter how good you feel, and even if you think your kidney transplant is working well, you should never (including years after your transplant) stop taking your anti-rejection medication. Stopping or missing anti-rejection medicine may cause a rejection to occur.
How should I take anti-rejection medication? Here are some tips to help you take your anti-rejection (immunosuppressant) medication as directed. Make taking your medicine part of your daily routine. Use digital alarms, alerts or apps to remember when to take your medication. Be creative because it is easy to forget, especially once you are feeling well. Know the name and dose of all of your medications. Understand the reason for taking each medication. Ask for and review all written instructions for any change in medication dose or frequency. Tell your transplant team of problems and concerns about medications during every clinic visit. If a doctor other than a member of your transplant team gives you a prescription, notify the transplant team before taking. Certain medications can interfere with your anti-rejection medications and keep them from working or cause their levels to increase to ‘toxic’ levels.
What medications can interfere with your anti-rejection medications and keep them from working? Herbal products, including herbal teas, marijuana and related cannabinoid (CBD) products can INTERFERE with your transplant medications. Over the counter medications can interfere with your anti-rejection medications. Always check with your transplant nephrologist.
Do anti-rejection medications have side-effects? Anti-rejection (immunosuppressant) medications have a number of possible side-effects which are usually manageable for most patients. Blood levels of anti-rejection medications will be checked regularly to prevent rejection and lessen side-effects. If side-effects do occur, your doctor may change the dose or type of medications.
What are the side-effects of anti-rejection medications? Some of the most common side-effects of anti-rejection medications include high blood pressure, diabetes, weight gain, and an increased susceptibility to some infections, and some forms of cancer.
What are the types of anti-rejection medications? There are 3 groups of anti-rejection (immunosuppressant) medications: (1) Induction agents – powerful anti-rejection medication used before the transplant in the operating room, and/or after the transplant surgery, while you are in the hospital; (2) Maintenance agents – anti-rejection medications you will take every day for as long as you have your transplanted kidney; (3) Rejection agents - medications which are used for the treatment for rejection episodes.
Rejection

Following a kidney transplant, rejection is a critical complication that can occur. You were not born with your transplanted kidney, so your body will recognize it as a “foreign” object and try to protect you by “attacking” or rejecting it. Your anti-rejection medications help you to combat this; however, you’ll have to do your part in taking them exactly as prescribed. You can also take other steps to help prevent rejection of a kidney transplant.
Tips to Prevent Rejection:
- Take your medication daily! Make it your duty to stay consistent and keep up with any medical changes your team prescribes.
- Continue to wear your mask and avoid being around sick persons and large groups of people. If you haven’t already, get vaccinated and keep up with CDC booster shot recommendations for Immunocompromised persons.
- Follow all dietary restrictions given by your nutritionist. Drink plenty of water to stay hydrated and avoid food high in sodium, fat, and cholesterols.
- With your doctor's clearance, begin a daily exercise routine such as walking, biking, or a dance class. Staying physically active will be a key part in your healing.
- Speak up! Learn about signs of rejection/infection and communicate any concerns you have to your care team. You know your body better than anyone. If something doesn’t feel right, say something!
Infection
Anti-rejection medicines that help keep your body from rejecting your transplanted kidney also impact your immune response. This puts you at risk for developing infections. Treating any infections as early as possible is the best way to keep you and your transplanted kidney healthy. Exposure to diseases such as COVID-19, BK and CMV viruses, the flu or pneumonia can make you very sick. Receiving vaccines, as determined by your transplant team, can help you stay healthy.
The most effective ways you can protect yourself from infection are:
- Wash and sanitize your hands regularly.
- Practice good overall hygiene at home, especially around pets and young children.
- Avoid close contact with people who have contagious illnesses.
- Keep up with your recommended vaccinations since they will help protect you from infection.
- Practice safe food handling. For more information on safe food handling, go to USDA: Basics for Handling Food Safely.
- Take your medication! Outside of the immunosuppressants you take, you will be prescribed preventative anti-infective medications during the first post transplant year. These will help prevent you from the most common infections.
If you ever experience any of the following problems, you should report them to your doctor as soon as possible:
- Sores, wounds, or injuries that do not heal.
- Urinary tract infection (UTI) symptoms including the frequent urge to urinate, pain or burning when urinating, cloudy or reddish urine, or bad smelling urine.
- Respiratory infection symptoms such as cough, nasal congestion, runny nose, sore or scratchy throat, especially if accompanied by fever.
- A temperature over 100 degrees.
Inform your doctor well in advance of any travel plans, especially if you plan on travelling outside of the country.
Infection
Anti-rejection medicines that help keep your body from rejecting your transplanted kidney also impact your immune response. This puts you at risk for developing infections. Treating any infections as early as possible is the best way to keep you and your transplanted kidney healthy. Exposure to diseases such as COVID-19, BK and CMV viruses, the flu or pneumonia can make you very sick. Receiving vaccines, as determined by your transplant team, can help you stay healthy.
The most effective ways you can protect yourself from infection are:
- Wash and sanitize your hands regularly.
- Practice good overall hygiene at home, especially around pets and young children.
- Avoid close contact with people who have contagious illnesses.
- Keep up with your recommended vaccinations since they will help protect you from infection.
- Practice safe food handling. For more information on safe food handling, go to USDA: Basics for Handling Food Safely.
- Take your medication! Outside of the immunosuppressants you take, you will be prescribed preventative anti-infective medications during the first post transplant year. These will help prevent you from the most common infections.
If you ever experience any of the following problems, you should report them to your doctor as soon as possible:
- Sores, wounds, or injuries that do not heal.
- Urinary tract infection (UTI) symptoms including the frequent urge to urinate, pain or burning when urinating, cloudy or reddish urine, or bad smelling urine.
- Respiratory infection symptoms such as cough, nasal congestion, runny nose, sore or scratchy throat, especially if accompanied by fever.
- A temperature over 100 degrees.
Inform your doctor well in advance of any travel plans, especially if you plan on travelling outside of the country.
Infection
Anti-rejection medicines that help keep your body from rejecting your transplanted kidney also impact your immune response. This puts you at risk for developing infections. Treating any infections as early as possible is the best way to keep you and your transplanted kidney healthy. Exposure to diseases such as COVID-19, BK and CMV viruses, the flu or pneumonia can make you very sick. Receiving vaccines, as determined by your transplant team, can help you stay healthy.
The most effective ways you can protect yourself from infection are:
- Wash and sanitize your hands regularly.
- Practice good overall hygiene at home, especially around pets and young children.
- Avoid close contact with people who have contagious illnesses.
- Keep up with your recommended vaccinations since they will help protect you from infection.
- Practice safe food handling. For more information on safe food handling, go to USDA: Basics for Handling Food Safely.
- Take your medication! Outside of the immunosuppressants you take, you will be prescribed preventative anti-infective medications during the first post transplant year. These will help prevent you from the most common infections.
If you ever experience any of the following problems, you should report them to your doctor as soon as possible:
- Sores, wounds, or injuries that do not heal.
- Urinary tract infection (UTI) symptoms including the frequent urge to urinate, pain or burning when urinating, cloudy or reddish urine, or bad smelling urine.
- Respiratory infection symptoms such as cough, nasal congestion, runny nose, sore or scratchy throat, especially if accompanied by fever.
- A temperature over 100 degrees.
Inform your doctor well in advance of any travel plans, especially if you plan on travelling outside of the country.
Infection
Anti-rejection medicines that help keep your body from rejecting your transplanted kidney also impact your immune response. This puts you at risk for developing infections. Treating any infections as early as possible is the best way to keep you and your transplanted kidney healthy. Exposure to diseases such as COVID-19, BK and CMV viruses, the flu or pneumonia can make you very sick. Receiving vaccines, as determined by your transplant team, can help you stay healthy.
The most effective ways you can protect yourself from infection are:
- Wash and sanitize your hands regularly.
- Practice good overall hygiene at home, especially around pets and young children.
- Avoid close contact with people who have contagious illnesses.
- Keep up with your recommended vaccinations since they will help protect you from infection.
- Practice safe food handling. For more information on safe food handling, go to USDA: Basics for Handling Food Safely.
- Take your medication! Outside of the immunosuppressants you take, you will be prescribed preventative anti-infective medications during the first post transplant year. These will help prevent you from the most common infections.
If you ever experience any of the following problems, you should report them to your doctor as soon as possible:
- Sores, wounds, or injuries that do not heal.
- Urinary tract infection (UTI) symptoms including the frequent urge to urinate, pain or burning when urinating, cloudy or reddish urine, or bad smelling urine.
- Respiratory infection symptoms such as cough, nasal congestion, runny nose, sore or scratchy throat, especially if accompanied by fever.
- A temperature over 100 degrees.
Inform your doctor well in advance of any travel plans, especially if you plan on travelling outside of the country.
Vaccines
Vaccines can protect you from developing certain infections. However, some vaccines that include live or weakened viruses can result in the development of those infections. Always check with your transplant team before receiving any vaccines or boosters. Read through our “Frequently Asked Questions” at the bottom of this section for a complete understanding of vaccines.

Vaccines

Vaccines can protect you from developing certain infections. However, some vaccines that include live or weakened viruses can result in the development of those infections. Always check with your transplant team before receiving any vaccines or boosters. Read through and print our “Frequently Asked Questions” at the bottom of this section for a complete understanding of vaccines.
What are some general rules for getting vaccines such as Hepatitis B, live vaccines, or a flu shot? You can get the Hepatitis B vaccine before transplant, but since it does not contain live virus, you can get it 3 months after transplant when your immunosuppression dose is lowered. Avoid all live vaccines. Avoid the nasal influenza vaccine. Wait at least 3-6 months after transplant before getting a flu shot; then get a yearly booster (injection only). Always consult with your Transplant team before getting any vaccines.
What if someone I know receives a live vaccine? You should avoid direct contact with anyone who has received a live vaccine. Examples include children who have received oral polio vaccine for 3 weeks, children who have received measles or mumps vaccines, adults who have received attenuated (weaker strength) Zostavax to prevent Varicella zoster (shingles), and children or adults who have received the nasal influenza vaccine.
What if I travel to another country? Contact your transplant physician if you plan to travel to another country. You may need to receive certain vaccines to prevent diseases that are common to the area.
Which vaccines are safe to get? The following vaccines are recommended: Diphtheria-pertussis-tetanus; Haemophilus influenzae B; Hepatitis A (for travel or other risk); HEPLISAV-B (a recombinant Hepatitis B vaccine); Pneumovax (single booster at 5 years); inactivated polio; Influenza types A and B (booster every year); Meningococcus (if at high risk); Shingrix for Varicella zoster; Typhoid Vi as well as the Pfizer-BioNTech, Moderna, and Johnson & Johnson/Janssen COVID-19 vaccines.
Which vaccines should I avoid? You should NOT receive the following “live” vaccines: Varivax (live Varicella zoster vaccine); Bacillus Calmette-Guerin (BCG); Smallpox; Intranasal influenza; Live oral typhoid Ty21a and other newer vaccines; Measles (except during an outbreak); Mumps, Rubella, or Oral polio; Live Japanese B encephalitis vaccine, or Yellow fever.
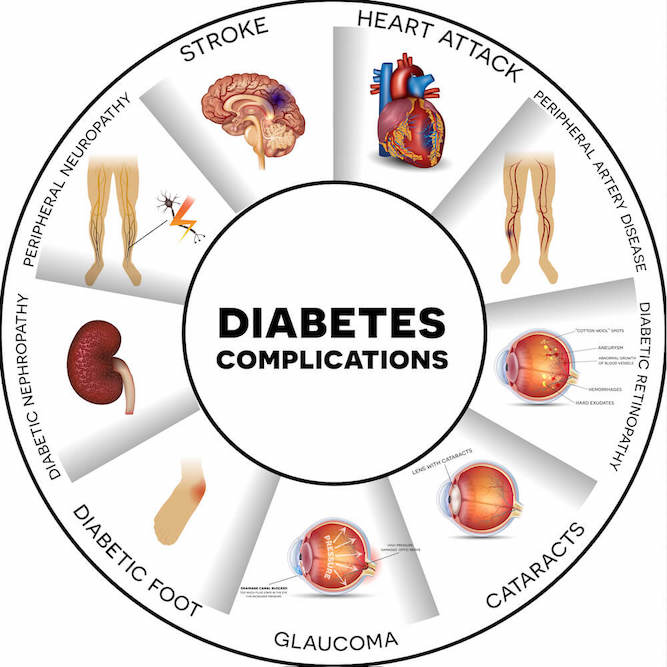
Potential Health Complications
There are potential health complications associated with transplantation that you should be aware of, but these should not discourage you from getting a transplant. A kidney transplant increases your chances for a longer, healthier, higher quality of life when compared to remaining on dialysis. You may already have some of these complications and be on medication to control them. Many of the conditions that you develop post-transplant can be successfully managed with diet and additional medications.
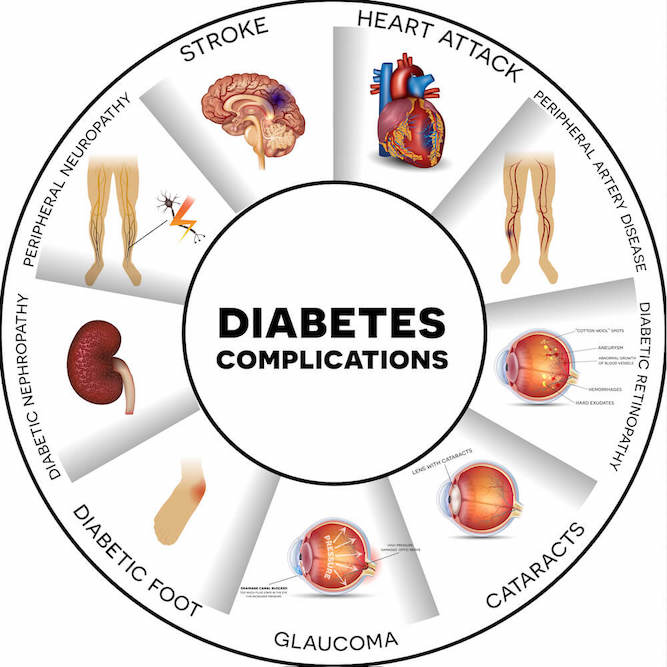
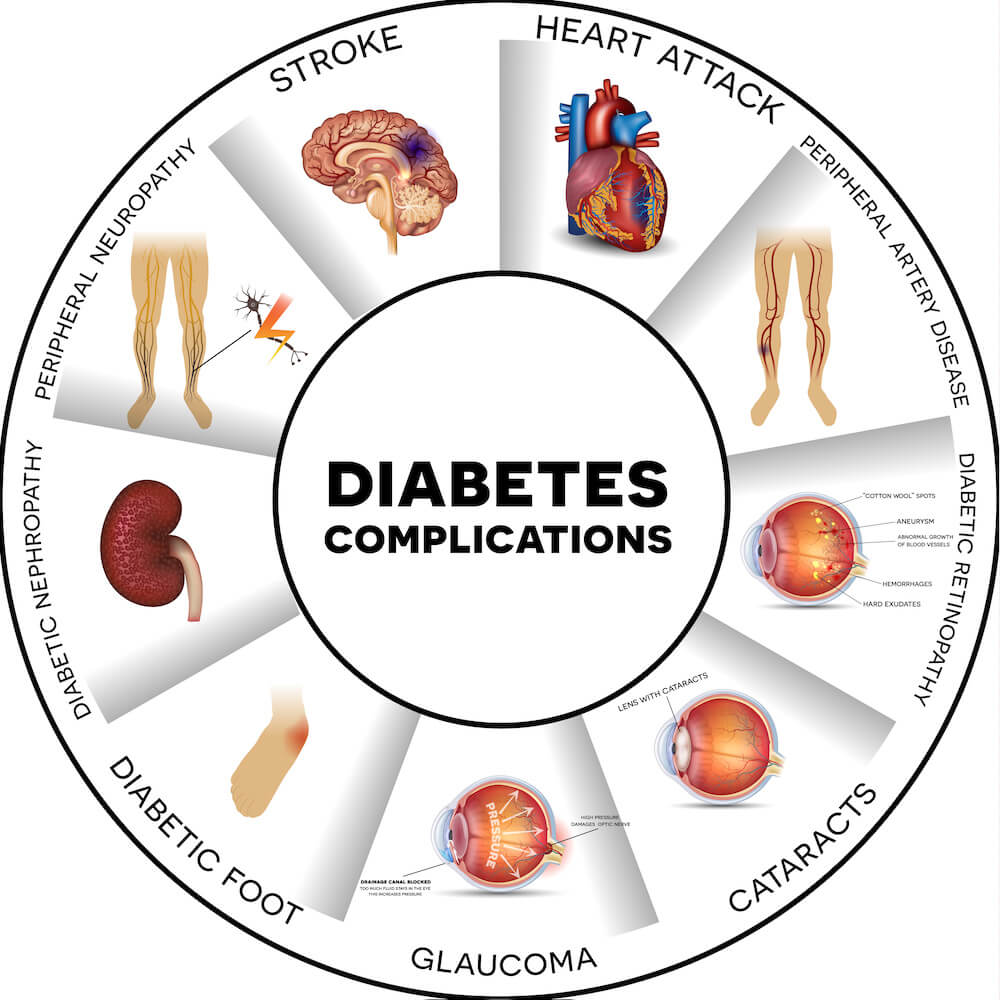
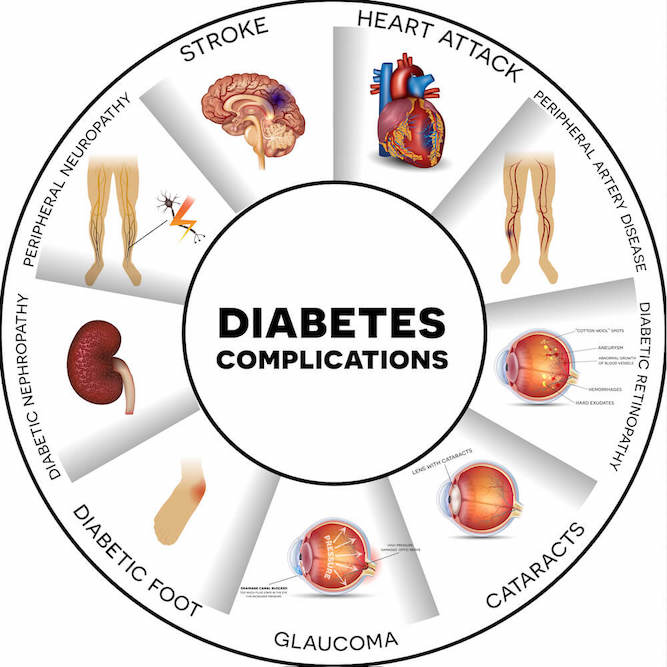
Diabetes
Even if you do not have a history of diabetes, it is possible to develop diabetes after a transplant. This can occur as a side effect of the medications you are taking to prevent rejection of your new kidney. The chances of having diabetes after transplant are higher for obese people. Those chances are also increased if others in your immediate family have diabetes (e.g., parents, brothers, sisters).
Having a high blood sugar can cause serious damage to your heart, blood vessels, eyes, feet, and nerves, as well as your kidney transplant. It only takes a few years of high blood sugars to damage your transplanted kidney.
Your blood sugar levels will be closely monitored by your care team after transplantation. If your doctors see fit, they will help you develop a plan to keep your blood sugar under control. High blood sugar is usually managed by eating a low carbohydrate diet, exercise (as allowed by your doctor), and diabetes medications.
Diabetes
Even if you do not have a history of diabetes, it is possible to develop diabetes after a transplant. This can occur as a side effect of the medications you are taking to prevent rejection of your new kidney. The chances of having diabetes after transplant are higher for obese people. Those chances are also increased if others in your immediate family have diabetes (e.g., parents, brothers, sisters).
Having a high blood sugar can cause serious damage to your heart, blood vessels, eyes, feet, and nerves, as well as your kidney transplant. It only takes a few years of high blood sugars to damage your transplanted kidney.
Your blood sugar levels will be closely monitored by your care team after transplantation. If your doctors see fit, they will help you develop a plan to keep your blood sugar under control. High blood sugar is usually managed by eating a low carbohydrate diet, exercise (as allowed by your doctor), and diabetes medications.
Diabetes
Even if you do not have a history of diabetes, it is possible to develop diabetes after a transplant. This can occur as a side effect of the medications you are taking to prevent rejection of your new kidney. The chances of having diabetes after transplant are higher for obese people. Those chances are also increased if others in your immediate family have diabetes (e.g., parents, brothers, sisters).
Having a high blood sugar can cause serious damage to your heart, blood vessels, eyes, feet, and nerves, as well as your kidney transplant. It only takes a few years of high blood sugars to damage your transplanted kidney.
Your blood sugar levels will be closely monitored by your care team after transplantation. If your doctors see fit, they will help you develop a plan to keep your blood sugar under control. High blood sugar is usually managed by eating a low carbohydrate diet, exercise (as allowed by your doctor), and diabetes medications.
Diabetes
Even if you do not have a history of diabetes, it is possible to develop diabetes after a transplant. This can occur as a side effect of the medications you are taking to prevent rejection of your new kidney. The chances of having diabetes after transplant are higher for obese people. Those chances are also increased if others in your immediate family have diabetes (e.g., parents, brothers, sisters).
Having a high blood sugar can cause serious damage to your heart, blood vessels, eyes, feet, and nerves, as well as your kidney transplant. It only takes a few years of high blood sugars to damage your transplanted kidney.
Your blood sugar levels will be closely monitored by your care team after transplantation. If your doctors see fit, they will help you develop a plan to keep your blood sugar under control. High blood sugar is usually managed by eating a low carbohydrate diet, exercise (as allowed by your doctor), and diabetes medications.
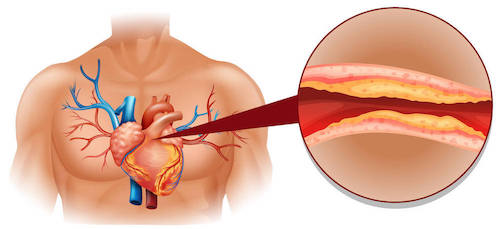
Heart Disease
If you’ve recently had a transplant, you are at risk of getting heart disease. Some risk factors (conditions) for developing post-transplant heart disease include smoking, diabetes, being overweight, hypertension (high blood pressure), high cholesterol, and spending a number of years on dialysis.
Some important things for you to do now to lower your chances of getting heart disease later are:
- Control high blood pressure
- Manage cholesterol
- Stop smoking
- Exercise, as allowed by your doctor
- Maintain a healthy weight by following a healthy diet
- If you have diabetes, work to keep it well controlled

Heart Disease
If you’ve recently had a transplant, you are at risk of getting heart disease. Some risk factors (conditions) for developing post-transplant heart disease include smoking, diabetes, being overweight, hypertension (high blood pressure), high cholesterol, and spending a number of years on dialysis.
Some important things for you to do now to lower your chances of getting heart disease later are:
- Control high blood pressure
- Manage cholesterol
- Stop smoking
- Exercise, as allowed by your doctor
- Maintain a healthy weight by following a healthy diet
- If you have diabetes, work to keep it well controlled

Heart Disease
If you’ve recently had a transplant, you are at risk of getting heart disease. Some risk factors (conditions) for developing post-transplant heart disease include smoking, diabetes, being overweight, hypertension (high blood pressure), high cholesterol, and spending a number of years on dialysis.
Some important things for you to do now to lower your chances of getting heart disease later are:
- Control high blood pressure
- Manage cholesterol
- Stop smoking
- Exercise, as allowed by your doctor
- Maintain a healthy weight by following a healthy diet
- If you have diabetes, work to keep it well controlled
Heart Disease
If you’ve recently had a transplant, you are at risk of getting heart disease. Some risk factors (conditions) for developing post-transplant heart disease include smoking, diabetes, being overweight, hypertension (high blood pressure), high cholesterol, and spending a number of years on dialysis.
Some important things for you to do now to lower your chances of getting heart disease later are:
- Control high blood pressure
- Manage cholesterol
- Stop smoking
- Exercise, as allowed by your doctor
- Maintain a healthy weight by following a healthy diet
- If you have diabetes, work to keep it well controlled

High Blood Pressure
If you had high blood pressure before getting your new kidney, it may continue after your transplant. High blood pressure can also occur as a side-effect of anti-rejection medications, organ rejection and/or obesity (from weight gain after transplant).
It is important to get in the habit of checking your blood pressure regularly at home. The target blood pressure for people with a kidney transplant is less than 130/80. Keeping your pressure controlled is essential and can be done by monitoring your weight, exercising regularly (as approved by a doctor), maintaining a low salt diet, and staying consistent with blood pressure medications if prescribed.

High Blood Pressure
If you had high blood pressure before getting your new kidney, it may continue after your transplant. High blood pressure can also occur as a side-effect of anti-rejection medications, organ rejection and/or obesity (from weight gain after transplant).
It is important to get in the habit of checking your blood pressure regularly at home. The target blood pressure for people with a kidney transplant is less than 130/80. Keeping your pressure controlled is essential and can be done by monitoring your weight, exercising regularly (as approved by a doctor), maintaining a low salt diet, and staying consistent with blood pressure medications if prescribed.

High Blood Pressure

If you had high blood pressure before getting your new kidney, it may continue after your transplant. High blood pressure can also occur as a side-effect of anti-rejection medications, organ rejection and/or obesity (from weight gain after transplant).
It is important to get in the habit of checking your blood pressure regularly at home. The target blood pressure for people with a kidney transplant is less than 130/80. Keeping your pressure controlled is essential and can be done by monitoring your weight, exercising regularly (as approved by a doctor), maintaining a low salt diet, and staying consistent with blood pressure medications if prescribed.
High Blood Pressure
If you had high blood pressure before getting your new kidney, it may continue after your transplant. High blood pressure can also occur as a side-effect of anti-rejection medications, organ rejection and/or obesity (from weight gain after transplant).
It is important to get in the habit of checking your blood pressure regularly at home. The target blood pressure for people with a kidney transplant is less than 130/80. Keeping your pressure controlled is essential and can be done by monitoring your weight, exercising regularly (as approved by a doctor), maintaining a low salt diet, and staying consistent with blood pressure medications if prescribed.

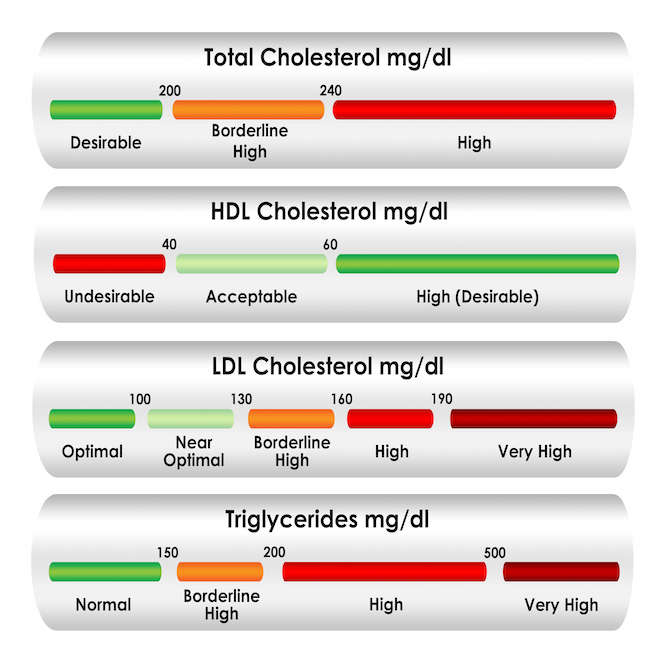
High Cholesterol and Blood Lipids
Many people develop higher cholesterol and lipid (fat) levels in the blood after transplant due to side effects from medication, weight gain, poor diet, family health history, and/or lack of exercise. Kidney damage that causes protein in the urine can also increase blood lipids. High blood lipids can clog blood vessels and increase your risk of heart disease and stroke.
Your doctor will help you manage your cholesterol and blood lipids. You can control high cholesterol and blood lipids by maintaining a heart healthy diet, exercising as allowed by your doctor, and taking any prescribed medications to lower your lipid levels.
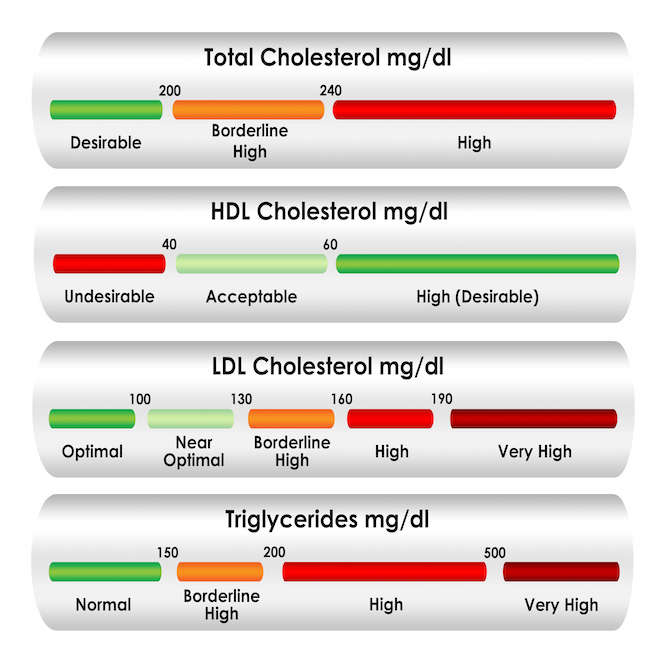
High Cholesterol and Blood Lipids
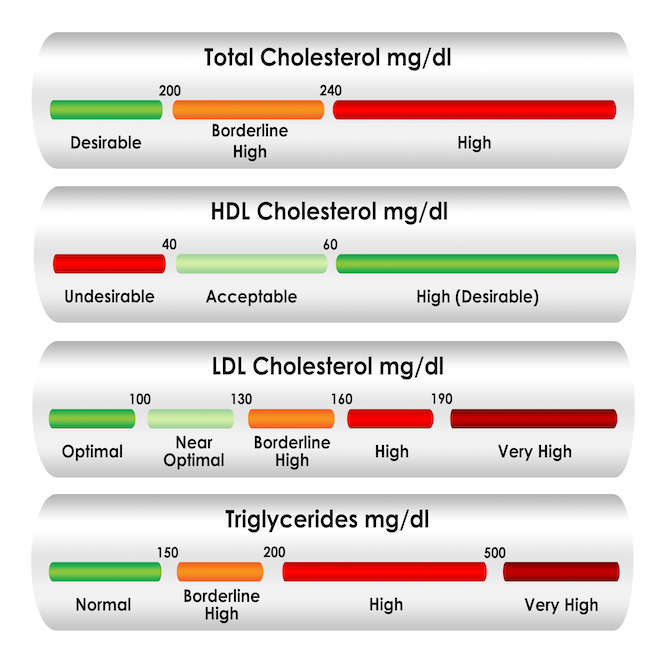
Many people develop higher cholesterol and lipid (fat) levels in the blood after transplant due to side effects from medication, weight gain, poor diet, family health history, and/or lack of exercise. Kidney damage that causes protein in the urine can also increase blood lipids. High blood lipids can clog blood vessels and increase your risk of heart disease and stroke.
Your doctor will help you manage your cholesterol and blood lipids. You can control high cholesterol and blood lipids by maintaining a heart healthy diet, exercising as allowed by your doctor, and taking any prescribed medications to lower your lipid levels.
High Cholesterol and Blood Lipids
Many people develop higher cholesterol and lipid (fat) levels in the blood after transplant due to side effects from medication, weight gain, poor diet, family health history, and/or lack of exercise. Kidney damage that causes protein in the urine can also increase blood lipids. High blood lipids can clog blood vessels and increase your risk of heart disease and stroke.
Your doctor will help you manage your cholesterol and blood lipids. You can control high cholesterol and blood lipids by maintaining a heart healthy diet, exercising as allowed by your doctor, and taking any prescribed medications to lower your lipid levels.
Smoking
Smoking cigarettes can damage your transplanted kidney and significantly increases your risk for heart disease, cancer, and lung disease. If you currently smoke, you are encouraged to stop.
Be sure to reach out to your transplant team for resources to help you quit. Your doctor can also provide you with medication to help you quit smoking if you have trouble quitting on your own. There are also online programs and Apps you may want to try. Here are some examples:

Smoking

Smoking cigarettes can damage your transplanted kidney and significantly increases your risk for heart disease, cancer, and lung disease. If you currently smoke, you are encouraged to stop.
Be sure to reach out to your transplant team for resources to help you quit. Your doctor can also provide you with medication to help you quit smoking if you have trouble quitting on your own. There are also online programs and Apps you may want to try. Here are some examples:
- BeTobaccoFree.gov
- NCI QuitPal App
(click on the links on the website)
Smoking
Smoking cigarettes can damage your transplanted kidney and significantly increases your risk for heart disease, cancer, and lung disease. If you currently smoke, you are encouraged to stop.
Be sure to reach out to your transplant team for resources to help you quit. Your doctor can also provide you with medication to help you quit smoking if you have trouble quitting on your own. There are also online programs and Apps you may want to try. Here are some examples:

Healthy Weight
You will likely gain weight after your kidney transplant. Weight gain after transplant is common due to medication side-effects, a less strict diet (as compared to the diet for dialysis), and a general increase of appetite. This can possibly lead to obesity, which increases the risk of heart disease and diabetes after transplant.
Your doctor and dietitian can help you develop a plan to keep a healthy weight that will involve exercise and healthy eating habits. There are also medical nutrition therapy services that your doctor can prescribe to provide you with nutrition counseling and information on managing lifestyle factors that affect your diet. Medicare and some commercial insurances cover these services.

Healthy Weight
You will likely gain weight after your kidney transplant. Weight gain after transplant is common due to medication side-effects, a less strict diet (as compared to the diet for dialysis), and a general increase of appetite. This can possibly lead to obesity, which increases the risk of heart disease and diabetes after transplant.
Your doctor and dietitian can help you develop a plan to keep a healthy weight that will involve exercise and healthy eating habits. There are also medical nutrition therapy services that your doctor can prescribe to provide you with nutrition counseling and information on managing lifestyle factors that affect your diet. Medicare and some commercial insurances cover these services.

Healthy Weight

You will likely gain weight after your kidney transplant. Weight gain after transplant is common due to medication side-effects, a less strict diet (as compared to the diet for dialysis), and a general increase of appetite. This can possibly lead to obesity, which increases the risk of heart disease and diabetes after transplant.
Your doctor and dietitian can help you develop a plan to keep a healthy weight that will involve exercise and healthy eating habits. There are also medical nutrition therapy services that your doctor can prescribe to provide you with nutrition counseling and information on managing lifestyle factors that affect your diet. Medicare and some commercial insurances cover these services.
Healthy Weight
You will likely gain weight after your kidney transplant. Weight gain after transplant is common due to medication side-effects, a less strict diet (as compared to the diet for dialysis), and a general increase of appetite. This can possibly lead to obesity, which increases the risk of heart disease and diabetes after transplant.
Your doctor and dietitian can help you develop a plan to keep a healthy weight that will involve exercise and healthy eating habits. There are also medical nutrition therapy services that your doctor can prescribe to provide you with nutrition counseling and information on managing lifestyle factors that affect your diet. Medicare and some commercial insurances cover these services.

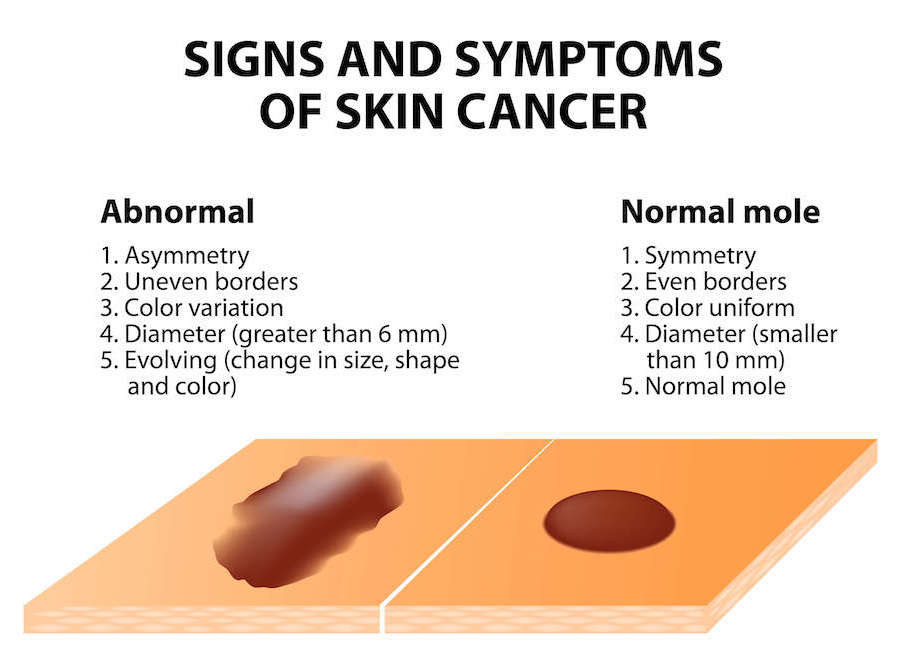
Cancer
As a transplant recipient, you have a higher incidence of developing cancer than the general population due to your anti-rejection medications. The medications decrease your immune function and the body's surveillance and defenses for certain types of cancer. The most common are melanoma (skin cancer) and lymphoma (white blood cell cancer). You can find further information on these and more types of cancers, symptoms to look out for, and prevention tips on the American Cancer Society’s webpage.
As a post-transplant patient, it is crucial that you keep up with your doctors’ visits and recommended exams. Women are encouraged to discuss the risks of cervical, breast, and colon cancer with their doctors. Men should discuss the risk of prostate and colon cancer with their doctors, as well.
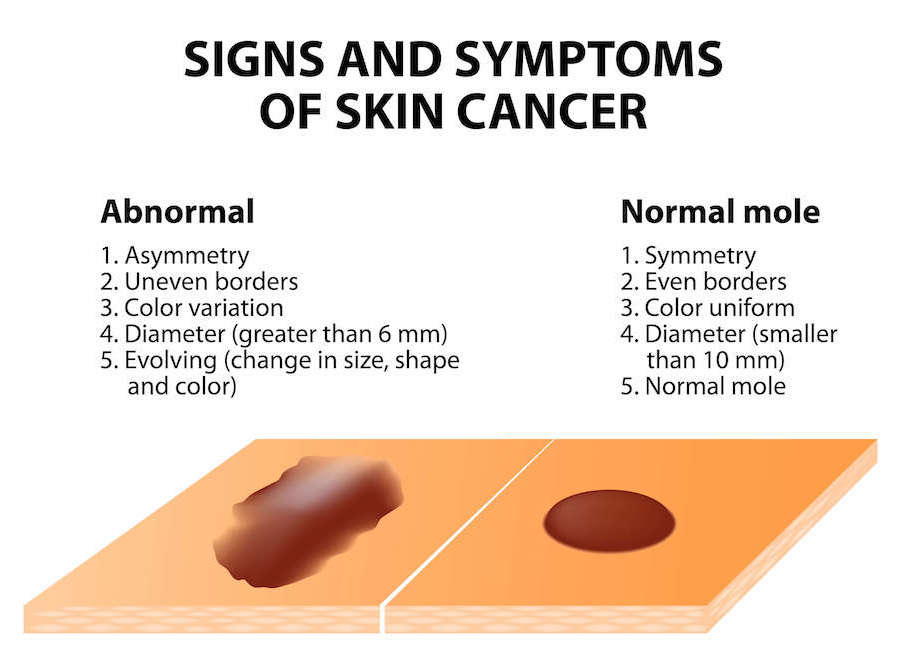
Cancer
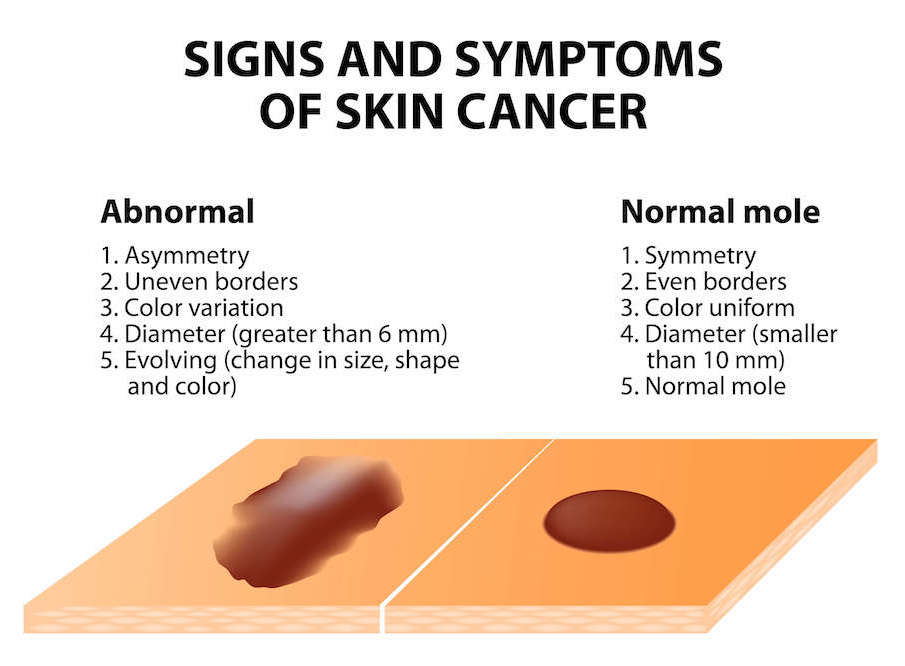
As a transplant recipient, you have a higher incidence of developing cancer than the general population due to your anti-rejection medications. The medications decrease your immune function and the body's surveillance and defenses for certain types of cancer. The most common are melanoma (skin cancer) and lymphoma (white blood cell cancer). You can find further information on these and more types of cancers, symptoms to look out for, and prevention tips on the American Cancer Society’s webpage (www.cancer.org).
As a post-transplant patient, it is crucial that you keep up with your doctors’ visits and recommended exams. Women are encouraged to discuss the risks of cervical, breast, and colon cancer with their doctors. Men should discuss the risk of prostate and colon cancer with their doctors, as well.
Cancer
As a transplant recipient, you have a higher incidence of developing cancer than the general population due to your anti-rejection medications. The medications decrease your immune function and the body's surveillance and defenses for certain types of cancer. The most common are melanoma (skin cancer) and lymphoma (white blood cell cancer). You can find further information on these and more types of cancers, symptoms to look out for, and prevention tips on the American Cancer Society’s webpage.
As a post-transplant patient, it is crucial that you keep up with your doctors’ visits and recommended exams. Women are encouraged to discuss the risks of cervical, breast, and colon cancer with their doctors. Men should discuss the risk of prostate and colon cancer with their doctors, as well.
Bone Disease
Bone disease (also known as chronic kidney disease-mineral and bone disorder or CKD-MBD) may develop or continue even after your kidney transplant. Bone disease can cause weak and brittle bones and increase your chance for fractures. CKD-MBD occurs due to medication side-effects, previous kidney disease, diabetes, smoking, lack of exercise, menopause, or being on dialysis for several years.
Your doctor will frequently check your bone health by testing your blood levels of calcium, phosphorous, parathyroid hormone (PTH), and Vitamin D. They may also ask you to obtain bone density measurements every few years after your transplant, which can lead to the prescription of medications to improve your bone density and prevent fractures.

Bone Disease
Bone disease (also known as chronic kidney disease-mineral and bone disorder or CKD-MBD) may develop or continue even after your kidney transplant. Bone disease can cause weak and brittle bones and increase your chance for fractures. CKD-MBD occurs due to medication side-effects, previous kidney disease, diabetes, smoking, lack of exercise, menopause, or being on dialysis for several years.
Your doctor will frequently check your bone health by testing your blood levels of calcium, phosphorous, parathyroid hormone (PTH), and Vitamin D. They may also ask you to obtain bone density measurements every few years after your transplant, which can lead to the prescription of medications to improve your bone density and prevent fractures.

Bone Disease

Bone disease (also known as chronic kidney disease-mineral and bone disorder or CKD-MBD) may develop or continue even after your kidney transplant. Bone disease can cause weak and brittle bones and increase your chance for fractures. CKD-MBD occurs due to medication side-effects, previous kidney disease, diabetes, smoking, lack of exercise, menopause, or being on dialysis for several years.
Your doctor will frequently check your bone health by testing your blood levels of calcium, phosphorous, parathyroid hormone (PTH), and Vitamin D. They may also ask you to obtain bone density measurements every few years after your transplant, which can lead to the prescription of medications to improve your bone density and prevent fractures.
Bone Disease
Bone disease (also known as chronic kidney disease-mineral and bone disorder or CKD-MBD) may develop or continue even after your kidney transplant. Bone disease can cause weak and brittle bones and increase your chance for fractures. CKD-MBD occurs due to medication side-effects, previous kidney disease, diabetes, smoking, lack of exercise, menopause, or being on dialysis for several years.
Your doctor will frequently check your bone health by testing your blood levels of calcium, phosphorous, parathyroid hormone (PTH), and Vitamin D. They may also ask you to obtain bone density measurements every few years after your transplant, which can lead to the prescription of medications to improve your bone density and prevent fractures.

Sexual Health and Fertility
Curious about your sexual health post-transplant? Most sexual functions will return after a successful transplant. You and your spouse or significant other should talk to your transplant team about any problems with sexual function or if you have questions about safe sex, contraception, or pregnancy. For women of childbearing age considering pregnancy, you should:
- Wait at least 1 year after your transplant and be sure your new kidney function is stable.
- See an obstetrician who specializes in high-risk pregnancies to evaluate and discuss the best course of care.
- Learn about the risks and benefits of breastfeeding. If you are interested in breastfeeding, it is crucial to review the medications you are taking with your obstetrician. Some medicines can be passed on through your breast milk and can be harmful to your baby.

Sexual Health and Fertility
Curious about your sexual health post-transplant? Most sexual functions will return after a successful transplant. You and your spouse or significant other should talk to your transplant team about any problems with sexual function or if you have questions about safe sex, contraception, or pregnancy. For women of childbearing age considering pregnancy, you should:
- Wait at least 1 year after your transplant and be sure your new kidney function is stable.
- See an obstetrician who specializes in high-risk pregnancies to evaluate and discuss the best course of care.
- Learn about the risks and benefits of breastfeeding. If you are interested in breastfeeding, it is crucial to review the medications you are taking with your obstetrician. Some medicines can be passed on through your breast milk and can be harmful to your baby.

Sexual Health

Curious about your sexual health post-transplant? Most sexual functions will return after a successful transplant. You and your spouse or significant other should talk to your transplant team about any problems with sexual function or if you have questions about safe sex, contraception, or pregnancy. For women of childbearing age considering pregnancy, you should:
- Wait at least 1 year after your transplant and be sure your new kidney function is stable.
- See an obstetrician who specializes in high-risk pregnancies to evaluate and discuss the best course of care.
- Learn about the risks and benefits of breastfeeding. If you are interested in breastfeeding, it is crucial to review the medications you are taking with your obstetrician. Some medicines can be passed on through your breast milk and can be harmful to your baby.
Sexual Health and Fertility
Curious about your sexual health post-transplant? Most sexual functions will return after a successful transplant. You and your spouse or significant other should talk to your transplant team about any problems with sexual function or if you have questions about safe sex, contraception, or pregnancy. For women of childbearing age considering pregnancy, you should:
- Wait at least 1 year after your transplant and be sure your new kidney function is stable.
- See an obstetrician who specializes in high-risk pregnancies to evaluate and discuss the best course of care.
- Learn about the risks and benefits of breastfeeding. If you are interested in breastfeeding, it is crucial to review the medications you are taking with your obstetrician. Some medicines can be passed on through your breast milk and can be harmful to your baby.

Mental Health
It is not uncommon for patients to develop anxiety and depression following a kidney transplant. While a transplant is a wonderful gift, it comes with many new responsibilities and challenges. You may be overwhelmed by all the new changes that are happening to you following your transplant. It is completely normal to feel this way.
Depression and anxiety may stem from prior health problems, sleep disorders, or stress from the transplant itself. For example, it is normal to worry about the health of the living donor or the tragedy that the deceased donor’s family has felt. Some anti-rejection medications may also cause depression or mood swings until the dose is decreased.
Discussing these issues with your transplant team will help determine whether treatment is needed, and then they can plan the appropriate treatment to help you get through this period.

Mental Health
It is not uncommon for patients to develop anxiety and depression following a kidney transplant. While a transplant is a wonderful gift, it comes with many new responsibilities and challenges. You may be overwhelmed by all the new changes that are happening to you following your transplant. It is completely normal to feel this way.
Depression and anxiety may stem from prior health problems, sleep disorders, or stress from the transplant itself. For example, it is normal to worry about the health of the living donor or the tragedy that the deceased donor’s family has felt. Some anti-rejection medications may also cause depression or mood swings until the dose is decreased.
Discussing these issues with your transplant team will help determine whether treatment is needed, and then they can plan the appropriate treatment to help you get through this period.

Mental Health

It is not uncommon for patients to develop anxiety and depression following a kidney transplant. While a transplant is a wonderful gift, it comes with many new responsibilities and challenges. You may be overwhelmed by all the new changes that are happening to you following your transplant. It is completely normal to feel this way.
Depression and anxiety may stem from prior health problems, sleep disorders, or stress from the transplant itself. For example, it is normal to worry about the health of the living donor or the tragedy that the deceased donor’s family has felt. Some anti-rejection medications may also cause depression or mood swings until the dose is decreased.
Discussing these issues with your transplant team will help determine whether treatment is needed, and then they can plan the appropriate treatment to help you get through this period.
Mental Health
It is not uncommon for patients to develop anxiety and depression following a kidney transplant. While a transplant is a wonderful gift, it comes with many new responsibilities and challenges. You may be overwhelmed by all the new changes that are happening to you following your transplant. It is completely normal to feel this way.
Depression and anxiety may stem from prior health problems, sleep disorders, or stress from the transplant itself. For example, it is normal to worry about the health of the living donor or the tragedy that the deceased donor’s family has felt. Some anti-rejection medications may also cause depression or mood swings until the dose is decreased.
Discussing these issues with your transplant team will help determine whether treatment is needed, and then they can plan the appropriate treatment to help you get through this period.

Healthy Lifestyle
A healthy lifestyle after transplant is crucial for many reasons. Many conditions such as diabetes, high cholesterol, and high blood pressure can be improved through living a healthy lifestyle. A healthy lifestyle also helps bring about a feeling of wellness.
Your transplant team will help you make informed choices to develop and live a healthy lifestyle. You should:
- Return to your regular routine, such as work, school, or housework, when you are able.
- Increase physical activity with regular exercise. Check with your doctor before you start an exercise program.
- Eat a healthy diet. Kidney transplant recipients are encouraged to follow a Mediterranean, heart healthy diet. A dietitian can help you make appropriate heart healthy food choices.
- Lose weight, as needed, to reach and maintain a healthy weight. Consult with your dietitian and transplant team for a healthy weight loss diet. Fad diets should be avoided. Once you get to your ideal body weight, you may feel even better.

Healthy Lifestyle

A healthy lifestyle after transplant is crucial for many reasons. Many conditions such as diabetes, high cholesterol, and high blood pressure can be improved through living a healthy lifestyle. A healthy lifestyle also helps bring about a feeling of wellness.
Your transplant team will help you make informed choices to develop and live a healthy lifestyle. You should:
- Return to your regular routine, such as work, school, or housework, when you are able.
- Increase physical activity with regular exercise. Check with your doctor before you start an exercise program.
- Eat a healthy diet. Kidney transplant recipients are encouraged to follow a Mediterranean, heart healthy diet. A dietitian can help you make appropriate heart healthy food choices.
- Lose weight, as needed, to reach and maintain a healthy weight. Consult with your dietitian and transplant team for a healthy weight loss diet. Fad diets should be avoided. Once you get to your ideal body weight, you may feel even better.
Healthy Lifestyle
A healthy lifestyle after transplant is crucial for many reasons. Many conditions such as diabetes, high cholesterol, and high blood pressure can be improved through living a healthy lifestyle. A healthy lifestyle also helps bring about a feeling of wellness.
Your transplant team will help you make informed choices to develop and live a healthy lifestyle. You should:
- Return to your regular routine, such as work, school, or housework, when you are able.
- Increase physical activity with regular exercise. Check with your doctor before you start an exercise program.
- Eat a healthy diet. Kidney transplant recipients are encouraged to follow a Mediterranean, heart healthy diet. A dietitian can help you make appropriate heart healthy food choices.
- Lose weight, as needed, to reach and maintain a healthy weight. Consult with your dietitian and transplant team for a healthy weight loss diet. Fad diets should be avoided. Once you get to your ideal body weight, you may feel even better.

Schedule a virtual visit with a Wellness Ambassador here.